Introduction
We report our initial series of terminally ill cancer patients treated with radiosurgery to the pituitary gland to alleviate pain.
Methods
A fully automated rotating gamma ray unit was used to deliver a high dose of radiation (150Gy) using an 8 mm collimator to the neurohypophysis in 11 patients suffering from opioid-refractory pain deriving from cancer.
Results
From November 2016 to November 2018, 11 patients were treated, and 10 were eligible for follow-up evaluation. Pain from bone metastases was present in 70%; others suffered from neuropathic and visceral pain. The median survival was 119.7 days (range: 32 to 370). The visual analogue scale (VAS) was nine (7-10) and standardized to 10; eight patients (80%) responded. The average VAS at the time of response was three (range: 1-6), and the average time to response was 2.8 days (range: 2-5). In the first week, 40% of the patients categorized the result as ‘excellent’, 30% deemed the result ‘good’, and 20% reported the result as ‘poor’. One patient (10%) referred to the result as ‘regular’. Those who responded were able to reduce their medications by at least 25%. The one-month average VAS score was five (range: 1-6), 60% reported a ‘good’ effect, 20% reported ‘excellent’ results, and 20% had no response. Of the study participants, 60% maintained their level of medicine consumption at lower than baseline. At the end of life, five patients (50%) presented substantial pain, two (20%) never had a therapeutic effect, and three (30%) died without substantial pain. There were no clinical complications that could be attributed directly to the treatment.
Conclusion
Radiosurgery to the pituitary gland is effective and safe and warrants further investigation to understand its potential role in palliative care in cancer patients.
Introduction
Pain derived from cancer represents a heavy burden on patients, their families, and healthcare systems worldwide; even in economically advanced countries, refractory oncological pain is a challenge for palliative care [1-2]. Although there is no strict definition of ‘refractory pain’, some authors agree that chronic refractory pain in cancer is the persistent physical signs and symptoms associated with phenomena where surgical interventions, radiation, nerve blocks, physiotherapy, and opioids have failed (and are either not feasible or tolerated) [3]. These are terminally ill patients who are usually bedridden or whose mobility, daily activities, and quality of life are severely impaired directly by pain, sedation [1], or by the side effects caused by pain management treatments. Limited resource settings (as experienced in most of the world) impose a further toll on this set of patients among whom moderate to severe pain has been reported in more than half the population [4-5].
Hypophysectomy or induced lesions to the pituitary gland and the stalk have historically demonstrated adequate pain reduction in advanced cancer patients. Initially performed to prolong survival in hormonodependent metastatic cancer patients, more contemporary indications were focused mainly on alleviating pain [6-11]. The use of radiosurgery for this procedure dates to the studies by Hayashi and others who report attempts to alleviate pain in oncological and non-oncological patients. High levels (70% to 90%) of pain relief have been reported with apparently low complication rates [12-13]. There are current attempts to resurge this technique and to create randomized controlled trials to further validate its efficacy [14].
We report the first series of terminally ill patients that were treated for refractory oncological pain using stereotactic radiosurgery with a fully automated rotating gamma ray unit in a country categorized as a limited resource setting.
Materials & Methods
Patient selection
We conducted a prospective non-randomized trial of radiosurgical hypophysectomy for patients in palliative care suffering from cancer pain, refractory to opioid therapy in whom no reasonable alternative intervention therapy (such as surgery, radiation, or pain medication) was feasible. The trial was approved by the hospital’s ethical committee in November 2016. The inclusion criteria were patients with cancer-related pain categorized as severe (scoring 7-10) on the visual analog scale (VAS) despite the best medical algology practice and optimal opioid dosing, were 18 years or older with a life expectancy under six months, and their pain could derive from bone metastases or other organs affected by the disease. The cases were reviewed and approved by an ad-hoc committee that included a palliative care specialist and an algologist, oncologist, and radiation therapy and neurosurgery staff. The main endpoints of the study were the reduction of the VAS score by at least 50% and a reduction in opioid or pain medicine consumption.
Radiosurgical technique
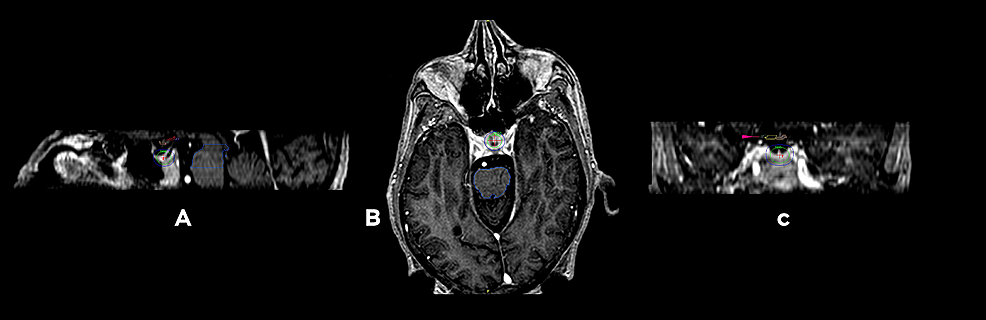
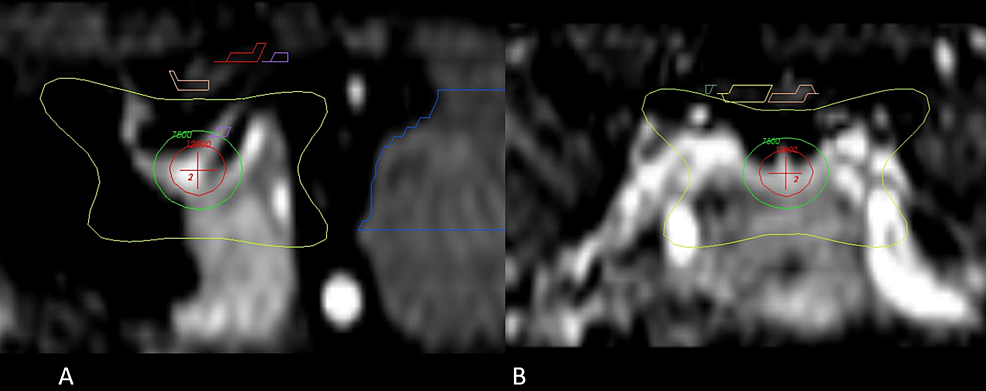
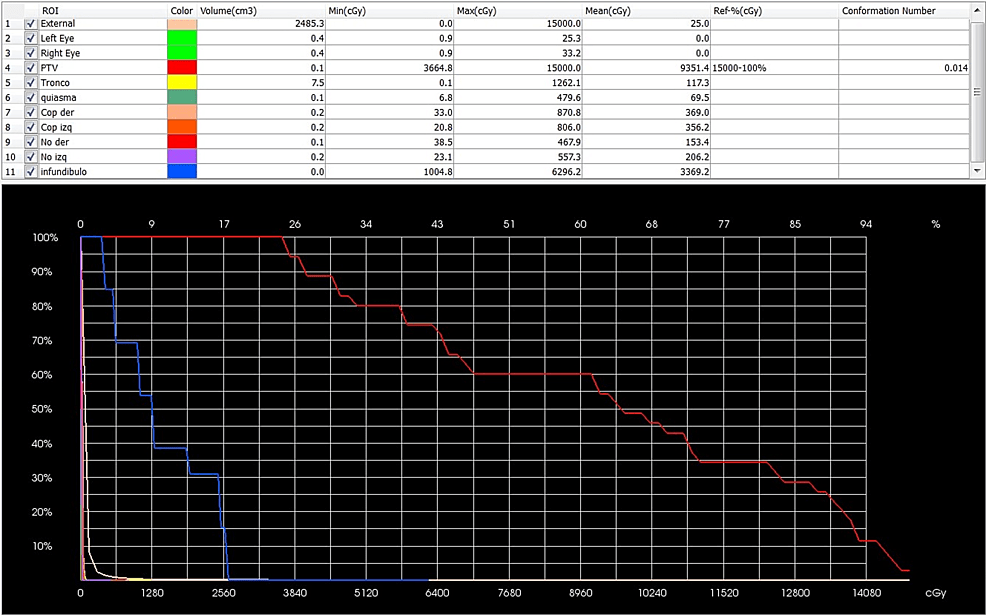
Patients fasted six hours on the day of the procedure and were prepared for sedation by the anesthesiologist using local anesthesia. An Infini stereotactic frame (Masep Medical Company, Shenzhen, China) was placed by a neurosurgeon, and the magnetic resonance imaging (MRI) acquisition was performed with a 1.5-tesla Avanto (Siemens Corporation. Erlangen, Germany). Normally, only one volumetric T1 of 1 mm to 1.5 mm slice thickness with no spacing of the head (apex to foramen magnum) was acquired; a contrast was added in one patient where metastatic lesions to the brain were also found. Images were transferred to the treatment planning station (TPS; Superplan; Masep Medical Company, Shenzhen, China). The organs at risk, which included the visual pathway and the brainstem, were contoured by neurosurgery; a single 8 mm collimator shot was placed to focus the isocenter of the shot on the neurohypophysis. Due to safety mechanisms specific to Superplan and the use of the prescribed high dose, we needed to place two shots in the same coordinates. The prescribed dose of 150 Gy to Dmax was administered to all patients with a gamma angle regularly fixed at 70°. The target was moved anteriorly or inferiorly as needed to comply with the organs at risk restrictions as stated by the American Association of Physicists in Medicine Task Group 101 Report [15] (Figures 1–3).
Patients did not receive more than 8 Gy as a threshold dose to more than 0.2 cc of the visual pathway. Patients did not receive a maximum point exceeding 10 Gy, nor did they receive over 10 Gy as a threshold dose to more than 0.5 cc of the brainstem or a maximum point exceeding 15 Gy.
Patient follow-up
Patients were contacted 72 hours after the procedure and every 15 days until the time of death. The VAS was standardized with patients and caregivers to 10 on the day of treatment to facilitate registry. Expected complications such as severe electrolytic variations, increased urine output, or visual disturbances were explained to caregivers as reasons to consult in case of an event. We used Wilcox signed rank test to determine p-values.
Results
From November 2016 to November 2018, 11 patients were enrolled and treated with radiosurgical hypophysectomy for intractable pain (Table 1); four patients had prostate cancer, four had breast cancer, two had cervicouterine cancer, and one had lung cancer. Eight study participants (72%) had multiple lesions and pain mainly emerging from bone, two had visceral pain from peritoneal shedding, and one had intractable combined neuropathic pain from brachial plexus involvement and metastatic disease. None of the patients were receiving any form of active treatment for their cancer given their advanced disease staging made them ineligible for treatment. One patient was lost to follow-up. Thus, the results from the remaining 10 were registered. All patients were receiving opioids (80% morphine injections, 20% opiate derivatives) at the time of treatment with a mean of daily medicine intake for pain at 12.5 times per day (range: 10 to 15 times per day), including antidepressants, neuromodulators benzodiazepine, and non-steroidal regular pain medicine.